Opioid Crisis
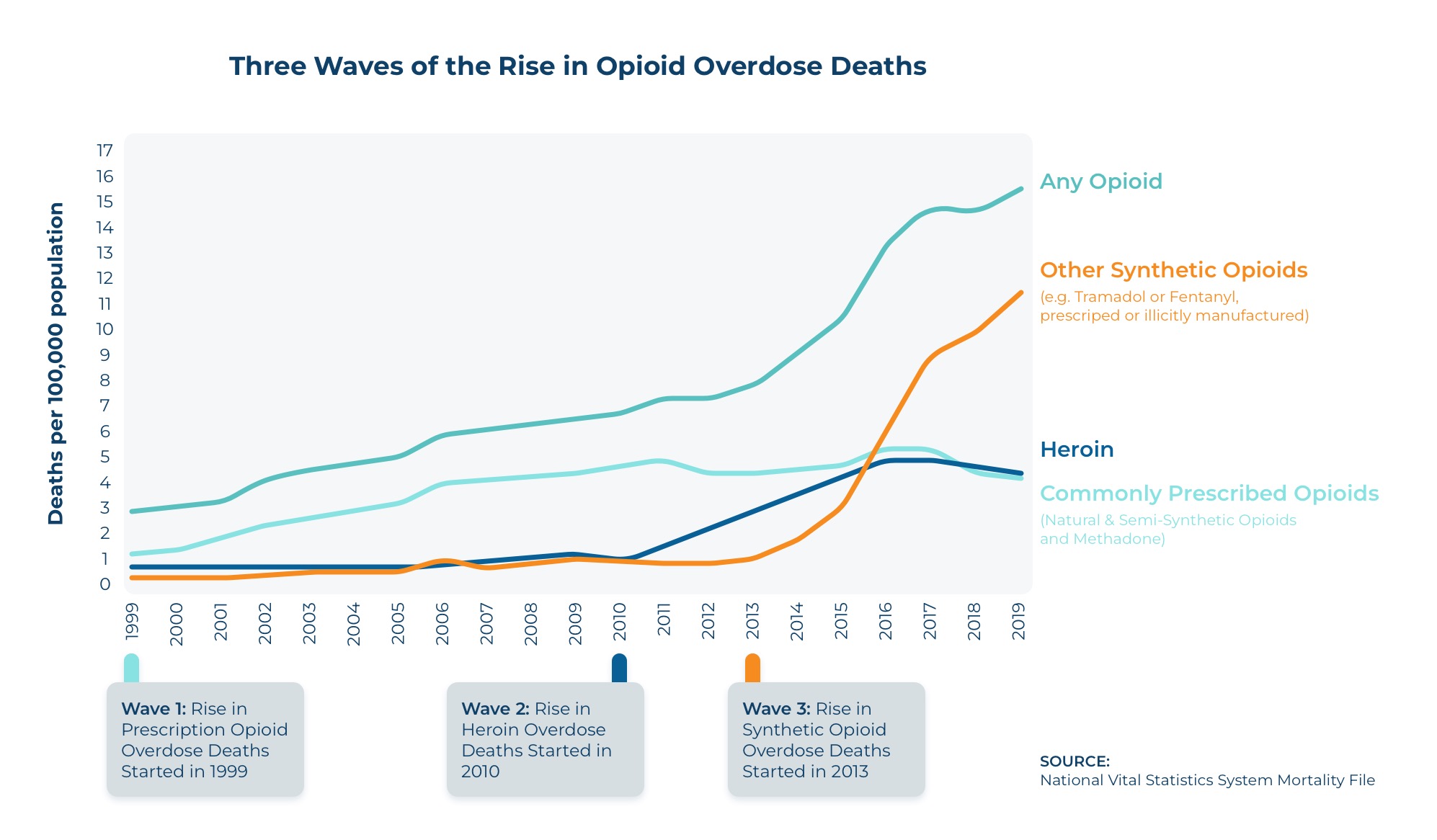
Recent studies from the CDC reveal a grim reality: in 2021 alone, opioids were responsible for 75% of the 107,622 drug overdose deaths in the United States.
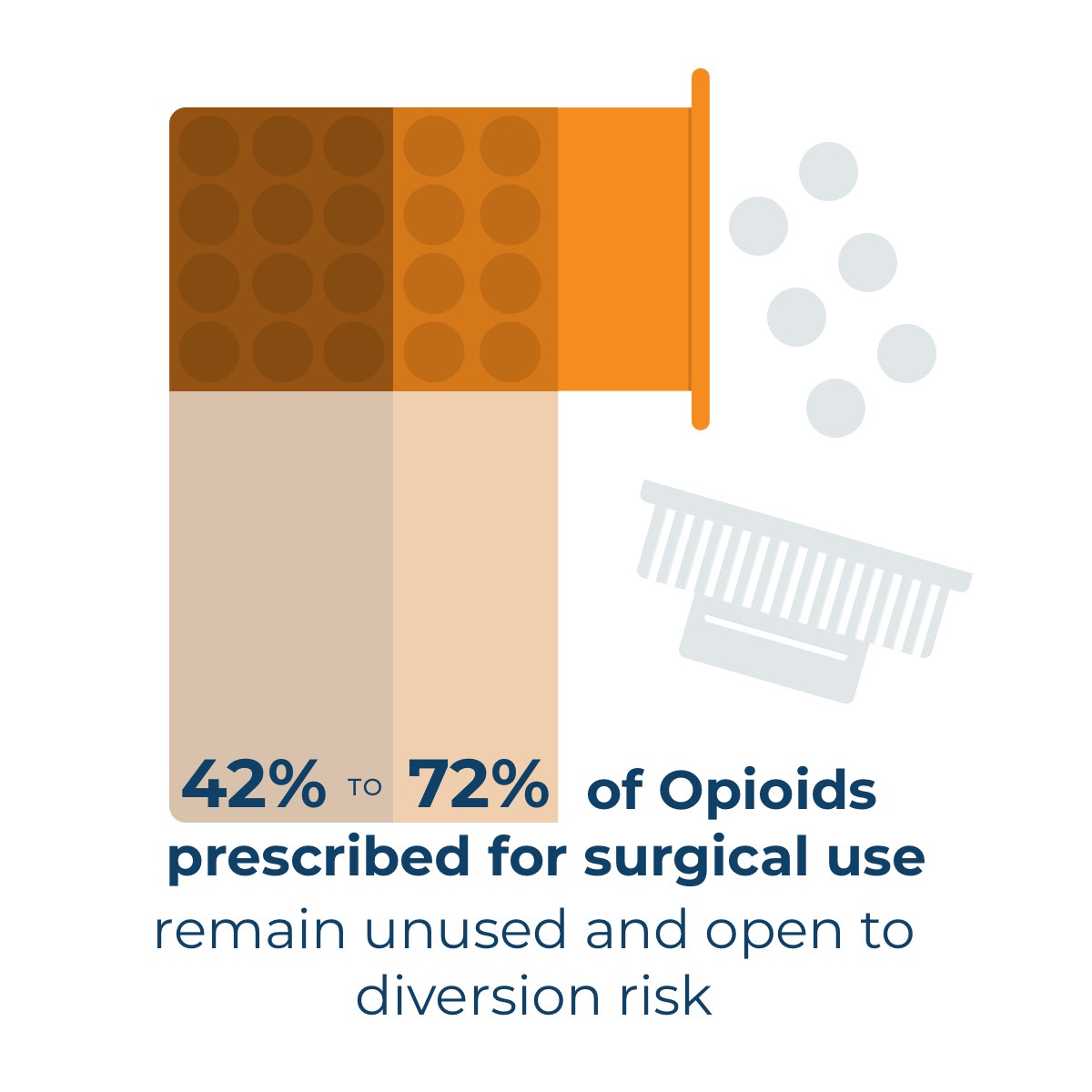
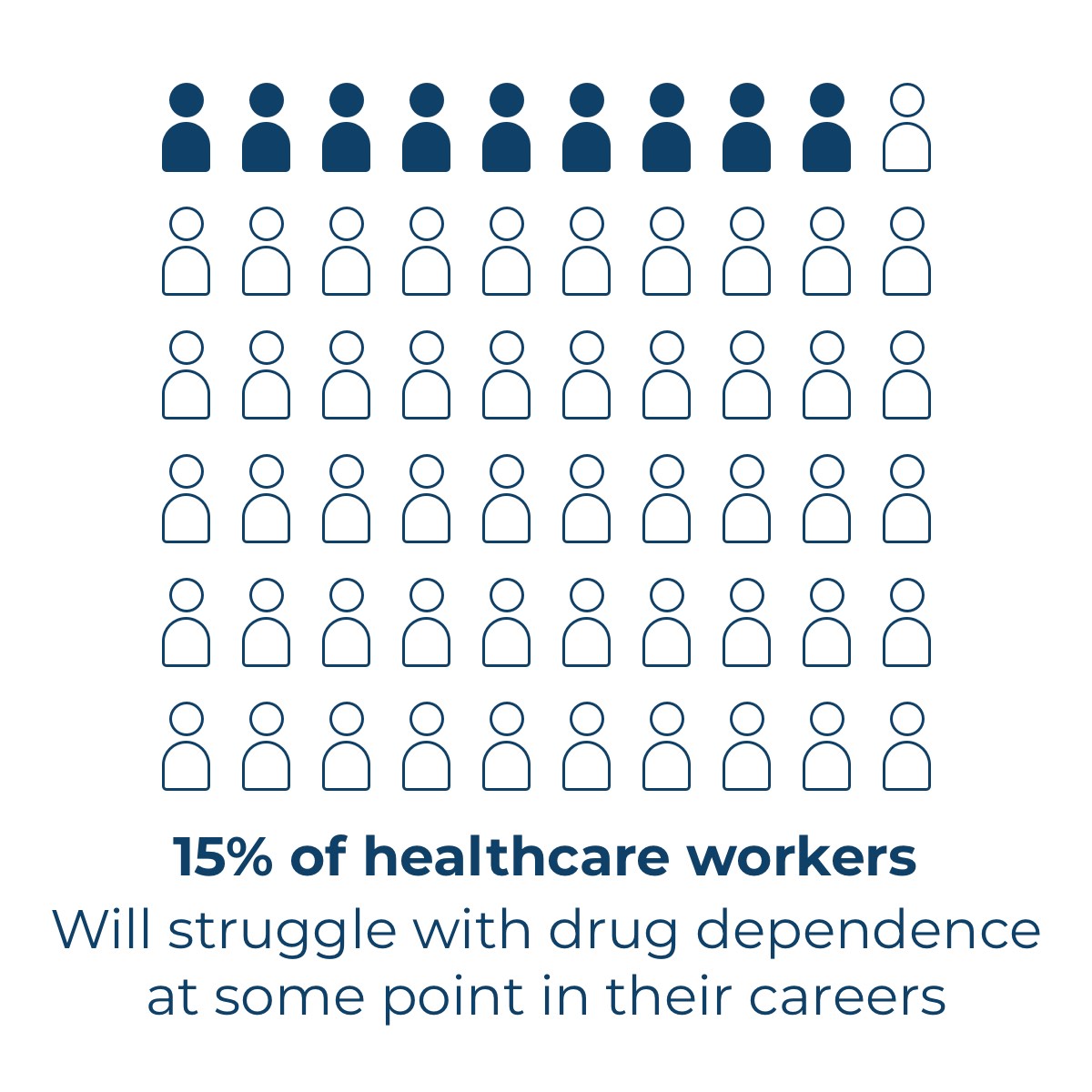
As health professionals, we are keenly aware of the opioid crisis. The problem is no longer a lack of attention to this epidemic, but rather, finding a solution and continuing education on how to spot and prevent drug abuse in the clinical environment. Keeping healthcare professionals at the forefront of our focus, we set out to design a product that was both simple and effective for opioid neutralization and disposal. Our goal was to develop a solution for drug diversion prevention that would be easy for health professionals to integrate into their already busy schedules.


What is drug diversion?
Drug diversion is when medication is used it was not intended. For instance, if person is prescribed main medication after surgery, but then uses it for recreational purposes, sells the substance or distributes it to other, the are participating in drug diversion. It can be difficult to identity, so education about the behavioral and physical signs of drug diversion is vital to helping nurses recognize it both in patients and among fellow medical professionals. Below we have listed “red flags” that can help in identifying a drug diversion.
Common practices for people participating in drug diversion:
- Stealing syringes or vials
- Under-dosing patients
- Replacing controlled substances with another product, such as saline
- Taking PRN medications from patients or pulling duplicate doses
- Creating false verbal orders
- Failing to waste or document waste, or raiding sharps containers.
Situations in the clinical environment that could point to drug diversion:
- Patients complaining of unrelieved pain or not receiving medications that have been documented as administered
- Drug-related items found in staff bathrooms or breakrooms
- Controlled medications with broken or unsecured caps or found in cabinets out of exterior packaging.
Behaviors of medical professionals in a clinical environment that suggest drug diversion involvement:
- Wasting complete doses, wasting no doses, or heavy drug wasting
- Failure to document waste
- Frequently wasting drugs that never reach the patient (dropped medications, patient refusal, discontinued orders)
- Repeatedly wasting with the same person as a witness (called a “waste buddy”)
- Repeatedly holding waste until the end of a shift or carrying medications in pockets
- Frequently asking colleagues to sign off on waste they didn’t witness
- Paying extra attention to or entering patients’ rooms who are receiving controlled substances
- Reviewing the medication orders of patients not assigned to them, helping colleagues medicate their patients, or volunteering to administer narcotics to patients
- Frequently asking for supplemental orders for controlled substances or pulling PRN medications
- Altering telephone or verbal medication orders
- Frequent charting or medication errors
- Sloppy documentation, omissions, and care inconsistencies
- Recurrent mistakes and poor judgment, variable work performance

Our Commitment
At Secure A Drug we are committed to keeping people safe by eliminating accessibility to unused drugs. Collaboration with and education of health care professionals on the signs of drug diversion and the importance of proper disposal of unused drugs is essential for success in preventing opioid overdose deaths. Together, we can better coordinate efforts to prevent opioid overdoses and deaths.

